I feel freaking amazing: a post-brain surgery update
Leaving UCSF neurosurgery on my own feet. Photo by Erika Dimmler.
Dear friends: I have been home from surgery for a few days and I feel amazing.
I am typing this post with no major assistance, so take this as a positive spoiler that my language and much of my proprioception skills survived this recent surgery. It could be the steroids talking, but I am incredibly happy and feel cognitively better than I did before surgery just a few days ago.
Words are flowing with no issues and no pauses, and I have a lot of strength. There are some left-right differences in balance and strength, but the differences are nothing compared to what I experienced six months ago. I know there are many weeks left to healing—and my face is a bit busted with the bruising and swelling—but if you didn’t tell me I had brain surgery six days ago I’d be ready to roll into work on Monday morning at full speed.
Below I recap what’s been happening, and share some of the high level details about my medical situation based on what we know right now. For those who can’t handle the long-form blogging, long story short: We are waiting for some information that will inform my treatment.
What’s been happening over the last few days 🚶
Neurosurgery at UCSF was on Tuesday, and Brett and I were headed home to Sacramento by Thursday at noon. That’s an insanely fast turnaround, and it is a good thing, because it means I am feeling awesome.
I was up and walking around the neurosurgery floor by 6pm on Tuesday night. I was offered a walker, didn’t feel like I needed it, but used it Tuesday night anyway. Come Wednesday morning I ditched the walker and took it easy on my own two feet. UCSF allowed me to leave the hospital on foot (no wheelchair) but they did want to see me get out the door with the walker. When I returned home Thursday afternoon, I walked a little over half a mile. On Friday I walked nearly 3 miles. On Saturday I walked 4 miles. I am strong and happy, and the hard part now is taking it easy.
My awake brain surgery, details about tumor resection… and why it was really cool
In the post I wrote before surgery I shared that the tumor was growing at a fast enough rate that my medical team was concerned and felt that an additional surgery was necessary—to remove tumor and help us understand how the tumor has changed so we could make treatment decisions.
I want to tell you about what we learned from surgery, but I can’t do it without also tell you about what it was like to have awake surgery. To me, both components are equally interesting and key to my experience.
What appears below is my “Liz-lay person” description of the surgery process, and is not a surgical report written by medical team. The text below is based from my memory from real-time events during surgery, and what was explained to me the day after surgery.
I tend to nerd-out about this stuff, so if it gets boring just jump to the boldface text as a cheat code. 🤓
-
During surgery, tissue was removed during an awake craniotomy through a continuous sampling process. After my surgeon resected pieces of tumor, tissue was immediately sent to a lab for analysis that was then reported back to the surgeon (and to me, because I was awake!) letting us know what they were finding.
The tumor tissue samples were all generally favorable—this was good news, but also not what we were expecting. We were expecting to learn that my tumor had progressed to a more aggressive grade. We knew there was still more to remove and learn, and on we went with surgery. My surgeon continued to resect all visible tumor, sending samples back to the lab for analysis, while also updating me about what was going on in real time.
-
As a brain tumor patient, and now researcher in this space, I am enrolled in a variety of studies of people with brain tumors. One of these studies, OPTIMUM (part of the Low Grade Glioma Registry), was ready and waiting for my fresh tissue to be packaged up and sent from UCSF to The Jackson Laboratory for additional analysis. Results from this analysis will be available in the coming weeks. I can’t wait to learn more.
-
But back to surgery… because, you know, I am still having brain surgery in this story…
While the tumor was being resected, my surgeon was also working to maintain my sensory and physical functioning. As a relatively healthy “young person” (I am still considered young in the brain tumor world) it is important to me that I be able to move, live, work, and play with no major impairment. My surgeon and I set goals in advance that there we certain side effects I would be OK living with—such as sensory loss—but other things I did not want to lose—such as damage to major motors areas.
-
With these goals in mind, the surgeon designed a novel way of having me move and react throughout surgery to make sure he was removing tumor tissue without injuring me. It is much more complicated and nuanced than I am able to explain here, but essentially the surgeon had me laying on my right side, while continuously moving my right leg and right arm in various movements. He would use an instrument to stimulate my brain to both voluntarily and involuntarily react to certain cues. It was not painful, and actually really interesting.
-
Throughout this process, the surgeon wore a headset microphone so I could hear every word he said, and I had a microphone and he could hear every word I said.
It was funny, actually, because there was a point when the microphone was cutting out and he asked his team to fix the audio, and he said, “Liz, can you check your microphone?” And I said, “Hey, hey, one, two, one, two. Liz on the microphone.”
I thought I was hilarious in the moment, but no one else laughed. I may have referred to someone on the anesthesiology team as a DJ. And now this is a fun story for myself and anyone else who might be laughing right now.
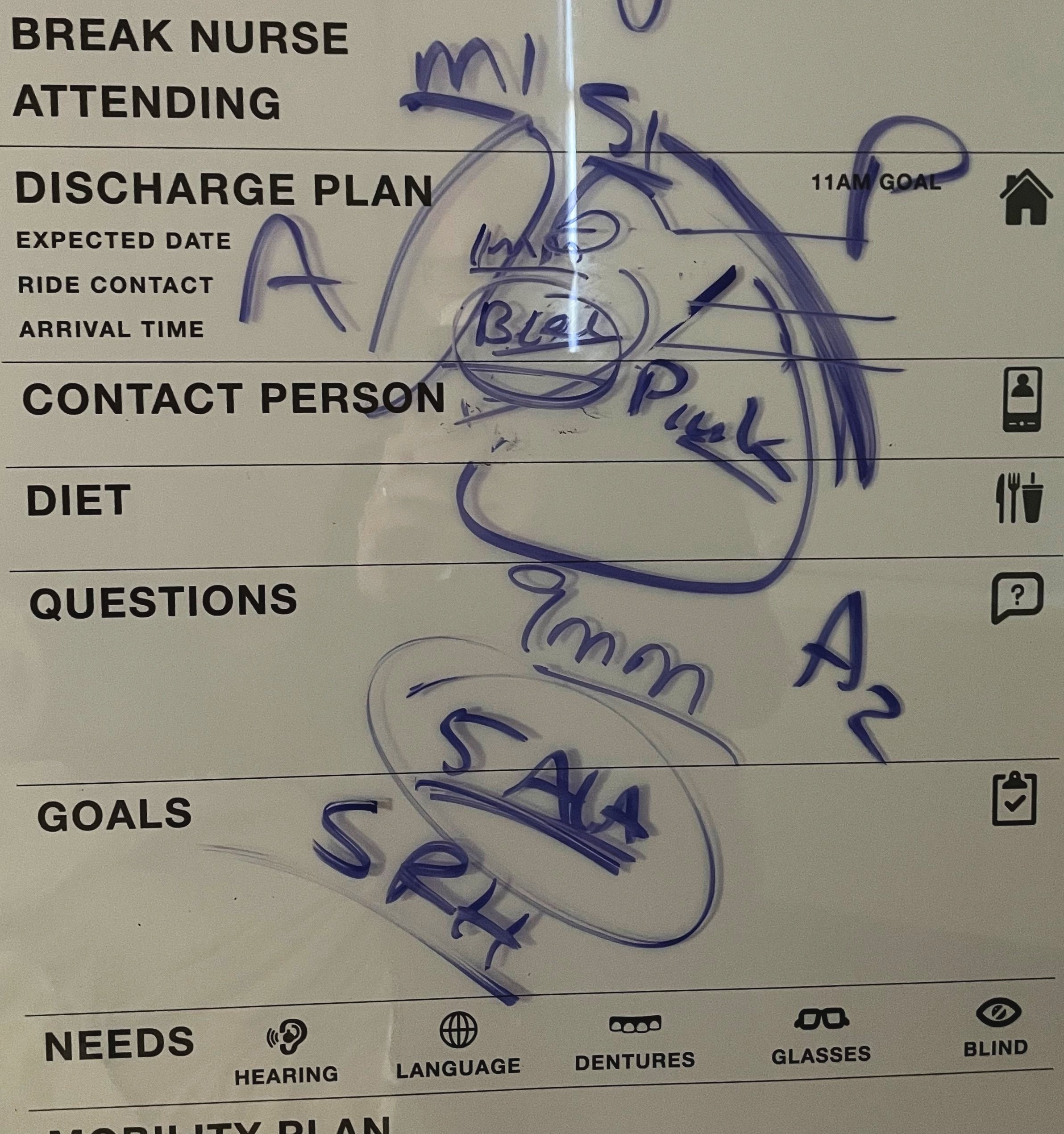
Some notes from the neurosurgeon on the whiteboard a few hours after surgery. Yes, somehow I understand what is being said here.
I could keep sharing the random moments from surgery that were cool and interesting, but for now I will jump ahead a bit.
What’s in the tumor, and what is my updated diagnosis? 🧠
The UCSF tumor board met Thursday. So far, they continue to see grade 2 astrocytoma—which is amazing, but also kind of unbelievable after 14 years of living with a malignant brain tumor. The tumor board decided to proceed with further analysis of the tissue; updated results will be available in the coming week(s). Additionally, my neuro-oncologist (brain cancer doctor) is contacting other top neuro-oncologists around the country for second (and third opinions) on both the pathology and how we might proceed considering what we know now.
My neuro-oncologist, Brett, and I believe it is the right and reasonable decision for me to move forward with targeted brain radiation at this time, most likely followed by chemotherapy. The timing of radiation and chemotherapy (and any bonus treatments associated with a clinical trial) are up for discussion. The good news is we have a few weeks to have these discussions and we don’t feel rushed in our decisions. This is a major a relief.
Brett’s quality of life is most important thing to me right now, and I can see the relief on his face.
The healing process ☢️
Even though I feel amazing right now, the plan is still for me to start some combination of radiation and chemotherapy in about four weeks. From what I know from all of my fellow brain tumor and cancer friends, radiation is grueling and fatiguing. I hear the first three weeks may feel not so bad, but the following three weeks are a lot, followed by a month of fatigue.
Next week Brett and I are meeting with a neuro-radiation oncologist at UC Davis Cancer Center, which is where I will be receiving some of my care. The UCSF and UC Davis doctors are working together as one team. I am especially looking forward to a referral to the UC Davis Cancer Center Supportive Oncology clinic, which helps with pain and symptom management. I am a big fan of palliative care, and am excited to finally qualify for this important level of care that is often not integrated into brain tumor care.
What’s next for friends? ❤️🩹
For local friends: The Meal Train is up and running a bit early. If you want to help us out, follow the Meal Train page. Thank you to Erika for handling this for us.
For far away friends: The Door Dash gift cards are handy! We have already been using them since we have returned home. Send Door Dash gift cards to: brettx209@yahoo.com.
***Update on gift cards for Lyft: I figured out the issue with gift cards through Lyft or Amazon for Lyft.
I learned Lyft can't hold >$300 in gift cards at one time.
I designed a spreadsheet to track anything beyond that amount, and confirmed at least one Amazon card worked.
I'll monitor the balance once radiation begins.
Between Lyft cards and local driving help, I think we have transportation covered and no additional gift cards are needed at this time.
Note: The Meal Train page includes options for local friends who want to give me a ride to the cancer center.
Major thanks
Clearly, I have much to share and I am pumped I can communicate in my own words, typing away with my own hands because last time was a much different experience. I hope to keep you all updated here, but in more frequent, short bursts on social media so you don’t have to read super long updates (except for the really important stuff).
I want to thank everyone who has been helping out in recent weeks and days, especially:
Leah and Ben: For giving Brett and I a place to stay in San Francisco. Leah is on the Board of Directors for National Brain Tumor Society and I can’t think of a better advocate to have in my corner at this time.
Erika: For coordinating the Meal Train and helping Brett and I with a speedy discharge from UCSF.
Dana: For running communications and handling my social media. At some point soon I will be ready to handle my own accounts, but I am not ready right now and she is an incredible ally.
Jennifer, Mel and Maya: In coordinating cat care while Brett and I were out of town, and continuing to help with errands.
Carlos: For helping Brett and I around the house and handling chores.